The patient, who suffered from a rare lung disease, started coughing up blood in late February. Admitted to the hospital overnight, she was told she needed to treat the condition or there could be a “bad outcome” the next time she started coughing.
She is, however, not treating the condition.
“I am 66 with preexisting cancer, so every contact I have with the health care system in this pandemic would put me at risk,” she says. “I threw the dice and decided to forgo treatment and take my chances at home.”
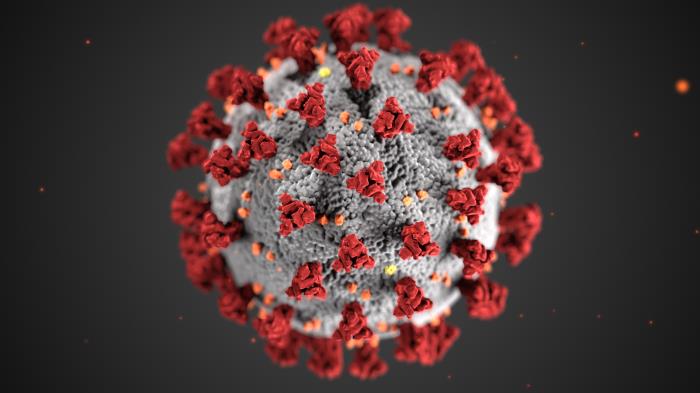
As hospitals focus on saving people at risk of dying from COVID-19 and other medical facilities shutter to avoid spreading the disease further, people with serious medical conditions or troubling health concerns are getting less care than they normally would. Doctors and dentists are seeing incomes contract because of the lower volume of appointments and procedures.
The combination raises questions not just about how New Yorkers’ health will suffer from the postponed appointments, deferred tests and delayed procedures, but also whether the medical industry will, ironically, contract in the midst of a pandemic or its aftermath.
There’s also the question of what happens when social distancing is eased and all that pent-up medical demand seeks service from a system where, depending on the nature of your needs, it was hard to get an appointment even before COVID put medical practices through a financial wringer.
Orders and advice to halt
Gov. Cuomo’s March 20 executive order restricting non-essential employees and businesses to remote operation exempted a large swath of medical work, including research and laboratory services, hospitals and walk-in-care health facilities.
But in a detailed order three days later, the state’s health commissioner, Howard Zucker, directed all hospitals to cease “non-essential elective surgeries and non-urgent procedures,” told ambulatory surgery centers to do the same, and suggested that doctors’ offices and others “reschedule unnecessary appointments and/or utilize telehealth modalities to provide care, to the greatest extent possible, in order to reduce potential exposure for our healthcare workforce as well as aid in social distancing.”
“If and when possible, elective and non-urgent surgeries that are cancelled throughout the COVID-19 response should receive priority scheduling upon return to normal operations,” Zucker’s order read. “DOH will notify you when normal operations may resume.”
The New York State Dental Association has made clear this applies to its members, too. “It is recommended that dental offices provide only emergency dental care for patients,” reads a notice on the NYSDA website.
Meanwhile, the Medical Society of the State of New York is publishing regular updates on emergency small-business loans for struggling practices—and postponed its annual House of Delegates meeting scheduled for this week in Tarrytown.
What’s essential?
It’s hard to quantify the health impact of the delayed patient care, because its different for each patient. Annual physicals could result in yet another wise—but not urgent—reminder to eat less sugar and exercise more, or can identify a more pressing health need. Surgery to fix varicose veins has a cosmetic impact, but also remedies a potentially serious circulatory problem.
“I had a regular cardiology check-up that had to be put off due to the crisis. It’s been rescheduled for April 22, but I doubt I’ll want to go anywhere near a hospital then and it will have to be postponed again,” says Ken Coughlin, a Manhattan resident. “I had a heart attack and a triple-bypass 12 years ago and get a twice-yearly checkup. I wouldn’t say it’s having much of an impact; my checkups have all been fine so I’m not too worried about waiting. On the other hand, I have an important urological exam in early June that will be more concerning if it has to be postponed.”
Certainly, patients receiving treatments that are known to be life essential are still being treated. “I’m continuing to receive chemo treatments, and thankfully have not had any major disruptions in the process,” says another New York City patient who asked not to be named and has breast cancer. “The only differences I experience are fewer persons scheduled for treatment (which is nice); having to speak with my oncologist by phone instead of face to face, and having to complete a pre-visit coronavirus questionnaire. Of course, all of this is expected given the crisis.”
The telehealth option
Some other patients are getting medical advice via telephone or video services. According to a spokeswoman, Planned Parenthood of Greater New York has scheduled more than 2000 virtual visits since the crisis began.
But long-distance healthcare is replacing a mere fraction of what occurred before. One New York City opthomologist estimates he’s seeing 10 percent of his normal patients, and doing 10 percent as much surgery as he would have. Dr. Mary Ruth Buchness, a dermatologist who heads the New York City Medical Society, says she is seeing two to three patients a day compared with 30 she would normally see.
Buchness says she knows of a doctor who claims to be doing 39 Zoom visits a day. “But in New York, patients won’t come out,” she says—and won’t get on the phone, even though she can deal with many conditions remotely.
Ideally, of course, she’d be able to touch and feel the problems patients have. She recently told a patient worried about cancer to feel whether the growth he’d detected was hard. It wasn’t. “Some patients need injections, so we temporize. I tell them other things to do.”
“When people are worried, they’re worried they have cancer. I’m able to tell them, ‘I don’t think it’s cancer. If it’s pre-cancerous, it can wait a couple months,’” she says. If anything looked like melanoma, she says, she’d escalate to an in-person appointment. Buchness says she knows an opthomalogist who is still seeing patients in person, but disinfects the entire office from top to bottom after each one, and therefore is seeing only one patient per hour.
‘Pretty shook up’
One patient who hasn’t found telehealth reassuring is Glenn Hudson, a 43-year-old Brooklynite and cancer survivor. In mid-March, he had a routine scan scheduled to make sure the cancer was not returning. COVID-19 was already breaking out. “It was kind of risky but I had to have the CAT-scan so I was just careful and went and did it,” he says. The doctors found no indication that the cancer had returned but did detect a blockage in his small intestine. They put him on a liquid diet and scheduled him for an MRI next week.
As wait times for imaging goes, that’s not a bad scheduling. The issue what’s been going on since then. “Sometimes I’ve been in pretty much excruciating pain,” Hudson said. “I didn’t necessarily stick to the liquid diet and I paid the price for it. If it hadn’t been for this situation we’re all in, I’d have definitely been in the ER then. It felt like something new is going on.” Usually, an intestinal blockage is an emergency-room issue, but doctors have told him to avoid that, Hudson says.
His own primary care physician isn’t doing telehealth at all. But Hudson has seen three doctors via telehealth and they’ve done little to reassure him about what he has been told is a “very rare, mysterious condition.”
“It’s not pretty. It’s not something to be taken lightly. I’m kind of a little bit shook up,” he says. His chief immediate worry is the “possibility of a puncture.” On a less serious but still significant level, being on a liquid diet during social distancing is rather isolating. Hudson feels he has to skip the dinner table so as not to be tempted to eat solids, but that’s painful to do when mealtimes with family are the hot social events of the day.
Worried about rent
Doctors like Buchness have different worry—keeping the lights on. When the crisis struck, “I thought, ‘I am dead. I am bankrupt. This business I built up is gone,’” she says. “I was in absolute terror.”
Since, she has applied for a federal small-business loan and recently received a $6,000 emergency grant from Medicare. She’s still employing an administrative aide; she now has enough cash to bring other staff back on but no active office to put them in. What’s more, “$6,000 doesn’t pay my rent,” she says.
Doctors generally get paid for work on about a two-month lag, which has served as a cushion for some practices in that it kept money coming in the door even though patients haven’t been. That same lag, however, could be a major problem when practices start up again with little cash to fund operations. What’s more, it’s unclear what practicing medicine will be like after COVID-19. Will specialist practices have to take people’s temperature when they come in the door? Will M.D.s have to wear masks during consultations?
As uncomfortable as it makes things for receptionists and other support staff, doctors can calibrate their spending on staff and other variable costs to their patient volume. But as is the case for other businesses, rent is an inescapable—and potentially very problematic—cost. When it comes to survival, Buchness says, “the landlord is key.” She adds: “I’m hoping they can forgive a month or something.”
Buchness doesn’t think doctors will be overwhelmed by a surge in demand once social-distancing is relaxed; if anything, a busy period would be a welcome change from the doldrums of the spring.
The American Medical Association tells City Limits it is considering the larger implications of the shutdown of most medical care this spring. But it doesn’t expect to have answers to the biggest questions anytime soon.