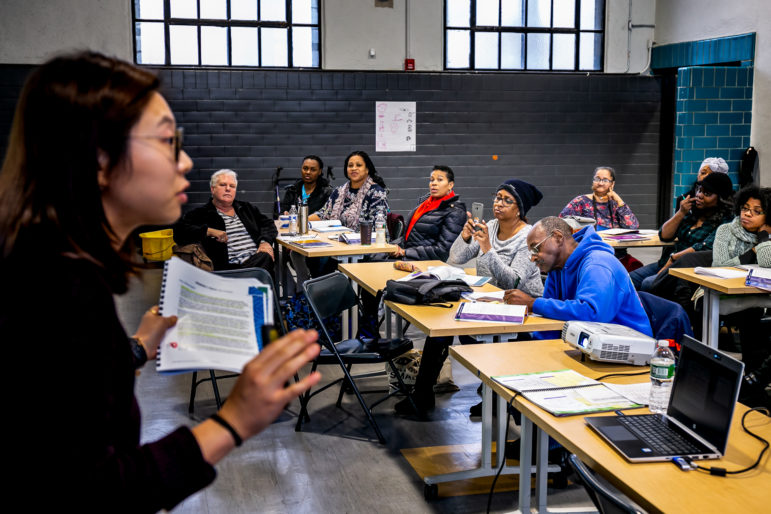
Adi Talwar
Jinny Jang conducting Thrive NYC’s Mental Health First Aid training class at the Highbridge Recreation Center in Manhattan. The day long program introduces participants to the unique risk factors and warning signs of mental health problems in adults over the age of 65.
When two suicides by seniors occurred within a year at Knickerbocker Village, a 1,590-apartment housing complex in the Two Bridges section of Manhattan’s Lower East Side, it rocked the community, says Councilmember Margaret Chin, who represents the 1st Council District where the complex sits.
In November of 2017, a terminally-ill Chinese community leader in his 60’s took his own life. Months later, in July of 2018, a 78 year-old former tenant association president and Vietnam veteran committed suicide.
Knickerbocker Village provides mental-health services for seniors through its Naturally Occuring Retirement Community, or NORC, an unplanned retirement community where senior services are funded through a combination of the city’s Department for the Aging (DFTA), New York State Department of Aging and City Council funds. Chin observed that the programs were helpful in the aftermath of the suicides.
“They were able to provide workshops to help seniors cope with that situation,” Chin says, including bilingual services for the building’s Chinese immigrant population.
Throughout the city, however, mental-healthcare funding and services are uneven at the city’s senior centers and NORCs, and neighborhood resources often determine what mental-healthcare seniors receive.
While Knickerbocker Village provides a range of services meant to facilitate community, including holiday celebrations and trips, many NORCs and senior centers lack funding for on-staff social workers, relying instead on caseworkers with less mental-health training who could be less likely to detect depression ahead of time.
In an effort to detect warning signs of mental illness in more of New York City’s seniors, Councilmember Diana Ayala introduced Intro 1180 last October, a bill that would mandate Mental Health First Aid training for caseworkers at all city-run senior centers and require a refresher course be taken every three years.
The trainings are meant to help anyone, regardless of previous mental-health training, detect signs of mental illness, provide immediate support and connection to more services. The city has already committed to training 250,000 New Yorkers in Mental Health First Aid over four years through the First Lady’s Thrive NYC Initiative, but no mandate exists for the training at senior centers, and not all senior center caseworkers have received the training.
New York has 27 NORCs and 249 city-run senior centers which are all managed by DFTA. Agency officials say that city-run Senior Centers – which provide a community hub for seniors – all have caseworkers who regularly screen every senior for mental health. And referrals are provided for outside care, according testimony from outgoing DFTA head Donna Corrado in her final City Council hearing on November 19.
But only 25 of those senior centers have more robust mental-health services through First Lady Chirlane McCray’s Thrive NYC initiative. Those services include a Geriatric Mental Health Initiative that facilitates clinician-led group conversations with residents centered around mental health and one-on-one therapy, as well as an in-home therapy program targeted to seniors called PEARLS and a Friendly Visiting Program that enlists volunteers to meet with seniors to combat isolation.
According to the American Psychological Association, 20 percent of older adults meet the criteria for a mental-health disorder, defined as a mental distress that interferes with life, family or work. Depression among older people might stem from losing loved ones, serious illness, or impairments in ability. And according to the CDC, the suicide rate for men over 85 is 45 per 100,000, well above the national rate of 11 per 100,000.
While New York City, through DFTA, has myriad services for the elderly, the growing size of the senior population – it is projected to grow from 1.1 million today to 1.4 million in 2040 – has lead to questions about how the city is connecting those services to those in need and recognizing warning signs when they occur.
“Most senior centers are under-resourced and don’t have the funding to hire licensed social workers that would be able to better pick up the signs, and so we want to ensure that everyone, specifically those that are coming in contact with our seniors regularly, are trained,” Ayala told City Limits of Intro 1180.
What is Mental Health First Aid?
Mental Health First Aid is a program, taught through an 8-hour course, meant to help trainees identify signs of mental illness and addiction and connect people who evidence symptoms of either problem with help. The program was developed in Australia, and is administered in the U.S. by the National Council for Behavioral Health, a D.C. based non-profit trade association that represents 2,500 community behavioral centers.
The Council says that from 2008, when it brought it the training to the U.S., until 2017, the program has grown to include 12,000 certified instructors and over 1 million people across the country have received training. The training is designed to address mental-health emergencies, like panic attacks or severe depressive episodes, giving attendees training to de-escalate someone from an extreme situation and, where, possible ferry them to more long-term care.
Bryan Gibb, director of public education for the National Council, says it’s useful to think of the training as like first aid or CPR, in terms of how it is administered and its focus on emergencies rather than long-term quality of life.
As with CPR or first-aid training, an individual can train to become an instructor and then take a standardized curriculum back to their community. Anyone can become an instructor by taking a week-long instructor certification course, and then can teach mental health first aid so long as they stick to the National Council’s method.
Mental Health First Aid could be particularly useful for senior populations because it helps break down a belief about mental health that is generational, Gibb says.
“Older adults often times have a lot of stigma associated with mental illness and they may elect not to seek help,” Gibb says. At minimum, the program is intended to get seniors to reach out to others about how they are feeling and refer them to professional help if they need it, he says.
Who has been trained?
Ayala’s legislation is intended to mandate training for caseworkers at city-run senior centers because, she says, caseworkers conduct most screenings and come into direct contact with seniors.
In a statement to City Limits, DFTA says that the number of caseworkers at their senior centers who have been trained in Mental Health First Aid is approximately 270 and that training is voluntary. But they pointed out that Mental Health First Aid, by its nature, is not intended just for specialized staff, many of whom have already received some level of mental-health training.
“Being trained in mental health first aid is not necessarily something that is exclusive to caseworkers,” says Zenovia Earle, a spokesperson for DFTA. She says that, to date, DFTA has trained nearly 5,430 staff to flag mental-health issues such as depression and substance abuse, a number that includes both Mental Health First Aid and other best practices.
“The Department for the Aging shares the City Council’s commitment to training frontline workers in Mental Health First Aid,” and is in the process of reviewing Ayala’s bill, Earle says.
Through Thrive NYC, the city has set an ambitious goal of training 250,000 residents in Mental Health First aid by 2021. To date, the city has trained 41,000 city employees across 14 city agencies in the practice, according to testimony by Myla Harrison, Assistant Commissioner of the Bureau of Mental Health.
Does it work?
The National Council says it doesn’t track data specific to Mental Health First Aid for seniors or know of any outside studies specific to older people. But other studies about Mental Health First Aid overall provide some evidence that the program helps with awareness. A Georgetown University study, for instance, found that 17 to 58 percent of participants reported using the training within three to six months of receiving it.
While studies can measure mental-health literacy among those who take the course, it is more challenging to measure whether the program is effective for those facing depression. Gibb says one data point they use is referrals to mental-health providers, a sign that a mentally ill person has followed up with a clinician specifically because of the program.
“It shows we’re moving people in the direction that they want,” Gibb says, but it’s an imperfect measure. “Mental Health First Aid is tricky because philosophically if we’re successful we don’t have anything to measure,” Gibb tells City Limits. “If early intervention is successful then it doesn’t lead to anything, because the issue is nipped in the bud.”
“That’s a hard thing to convince people who are giving you money,” Gibb quips. But the training regimen has been widely adopted:Pennsylvania’s Department of Corrections trained all 18,000 members of its correctional staff.In Rhode Island, a 2016 law mandated the training for all police officers.
‘Friendly Visiting’
According to DFTA, more than half (54 percent) people interviewed through its Geriatric Mental Health initiative at senior centers have an identifiable mental-health need or problem, such as depression, and about one in 10 screen positive for suicidal ideation.
While mental-health first aid is meant to flag issues in populations, the program presupposes that seniors have access to other long-term services.
“It’s not necessarily a long-term process,” Gibb says, noting that the program is meant to identify mental illness but not to follow a person through the arc of recovery.
The city has other longer-term programs that it uses to help seniors with quality of life. Among them is PEARLS, which stands for Program to Encourage Active Rewarding Lives. The program provides short-term in-home mental-health care for seniors, intended to give them tools to recognize their depression and change their thinking. It runs for six to eight sessions over a course of three to four months. Since the program was introduced in 2017, 638 older adults with depression have completed PEARLS treatment, according to testimony by Myla Harrison, Assistant Commissioner at the Bureau of Mental Health.
Despite the program’s popularity, clients have to wait to years to be readmitted to the program, something many seniors ask for.
“They love the program, and they just wish it was either longer. Sometimes it’s not even about the depression, they just enjoy speaking with someone,” says Martine, a program assistant for the Visiting Nurse Service of New York, or VNSNY, which administers the program in Manhattan and Queens. She declined to provide her full name.
Seniors hear about PEARLS through referrals from case managers, social workers, outside agencies and doctors. VNSNY also does outreach about the program in senior centers, and some seniors refer themselves.
If seniors are still looking for care, PEARLS administrators may recommend them to the city’s Friendly Visiting Program, a more long-term Thrive NYC program consisting of less formal in-home visits.
Visitors in this program check in on seniors at least twice a month to have more open-ended conversation and provide emotional support. Since the program’s inception volunteers have made over 17,170 visits consisting of over 27,200 hours, according to testimony by former DFTA head Corrado.
“The program model can provide connection to community, and may prevent the isolated senior from declining into depression and loneliness,” Corrado said in her testimony. All Friendly Visiting volunteers receive Mental Health First Aid training, Corrado noted.
Seniors who need more treatment will have to navigate Medicare and Medicaid, which present their own challenges and funding gaps. Medicare Part B covers outpatient mental health but is limited to only certain providers, and premiums start at $134 a month. New York State’s Medicaid expansion does not fund mental-health home visits, crucial for seniors who are less mobile than younger adults. DFTA says it helps seniors navigate those federal programs.
Thrive NYC and equity
DFTA notes that their Thrive NYC programming is open to all New York City seniors and not just residents of the 25 participating centers. They also provide other mental-health programs in all senior centers, such as bereavement groups when a senior passes, as well as Agetastic, a health promotion program that targets physical and mental health among seniors and touches on self-help tips like decluttering.
But the 25 senior centers that receive the more robust Thrive NYC programming represent less than 10 percent of city-run centers, which drew questions at the November 19 City Council meeting about how DFTA chose the centers.
When asked by about that by Ayala, outgoing DFTA head Corrado responded that the cooperating senior centers had been chosen carefully in cooperation with four nonprofit providers – JASA in The Bronx, Weill Cornell in Brooklyn and Staten Island, Community Advisory Program For The Elderly at the Samuel Field Y in Queens, and Service Program for Older People in Manhattan. The 25 Thrive NYC senior centers were determined, among other factors, by “calls from senior center providers that have a preponderance of very disturbed senior center members for whatever reason,” according to Corrado, which she acknowledged in her testimony was anecdotal.
“None of the identified senior centers are in communities that are necessarily impoverished,” Ayala said in the meeting, noting that her own South Bronx had seen a spike of depression in older women but that none of the Thrive NYC-affiliated senior centers had been centered there.
“I don’t see anywhere where it’s reflected what additional resources have been kind of steered in that direction,” Ayala added.
Corrado responded that mental health did not discriminate by income level, and that impoverished areas often had other mental health services embedded in the community, which Ayala said was not the case in the Council district she represents.
Program providers point out that expanding Mental Health First Aid training may be helpful, but will not meaningfully address equity.
“Having more training is a good thing, but to expect that it’s a panacea for all mental-health issues and that we’ll be able to treat all mental-health issues isn’t realistic,” says Alan Cohen, the chief health program officer at JASA, the Jewish Association Serving the Aging. The agency provides health services to 14 of the city’s NORCs and partners with Thrive NYC to administer PEARLS in the Bronx.
Cohen added that in addition to different levels of staffing at senior centers, many other inequities need to be resolved for seniors to get proper long-term mental-health care, including a serious lack of licensed, Spanish-speaking mental-health clinicians across the city.
As far as expanding Thrive NYC past the cooperating 25 senior centers, DFTA said that they are in conversation with the first lady about this possibility but are still evaluating the existing programming to gauge its success.
“We really need the evidence to show that the investment is worthwhile,” Corrado said in her testimony.
Ayala said she had difficulty finding a provider to bring Thrive NYC services to the South Bronx, and that a mental-health training she tried to organize was under-attended and had to be cancelled, which she attributed to senior center staff being underfunded and overworked.
She says this is part of the reason she is pushing for Intro 1180. A former senior services employee, Ayala likens it to the first aid training she was required to have when she worked with seniors.
“In the same way that we train for CPR, we should be training individuals in first aid on mental health, and we’re not doing that at the senior center level,” Ayala said.
Amy Chaffy, a Chief Program Officer at JASA, says any mandate should be sensitive to the budget and workload of senior center employees. “It’s a balancing act in terms of what we expect of staff,” she says. “But the aging population is growing, and the incidence of mental-health issues will increase as that population grows, so to effectively link people to services is a valuable direction to go in.”
Editor’s Note: This article has been corrected to remove a reference to PEARLS being based in senior centers (it is a home-based program) and to note that the Geriatric Mental Health initiative includes one-on-one therapy as well as group sessions. For clarity, we have added mention of DFTA’s assisting seniors navigating Medicare and Medicaid.

Support for this article was provided by Rise Local, a project of New America NYC.









3 thoughts on “Do NYC’s Seniors Need More Mental Health First Aid?”
Pingback: The Need For Expanded Mental Health First Aid for Senior Citizens - This Is The Bronx
Well described!! Keep up the good writing.
Great explanation. I love your content it is valuable and very informative. Thank You.